From sinardaily.my
Chronic workplace stress doesn’t just stay bottled up in your headspace. Instead, it manifests physically, particularly through your skin
YOU'RE smashing deadlines, answering emails beyond working hours and surviving on caffeine and sheer willpower. Your brain might be putting on a brave face, but your skin might be staging a silent protest.
That mysterious breakout, persistent rash, or sudden flare-up that seems to be immune to every serum might not just be a skincare issue, it could be your job waving a red flag.
It turns out, stress at the workplace could be doing more than fraying your nerves—they’re potentially wreaking havoc on your largest organ: your skin. According to dermatologist Dr Felix Yap Boon Bin from Sunway Medical Centre, your body is not shy about showing you when it’s had enough.
When contacted by Sinar Daily, Dr Felix shared how chronic workplace stress doesn’t just stay bottled up in your headspace. Instead, it manifests physically—particularly through your skin—with conditions ranging from acne and rosacea to eczema, psoriasis, acne vulgaris, rosacea, eczema, psoriasis, systemic lupus erythematosus, scalp folliculitis, and seborrheic dermatitis, thus demanding a clinic or hospital visit.
This is because he said that chronic workplace stress could contribute to hormonal changes, such as elevation of cortisol levels in the body, aside from interference of the sex hormones, including testosterone and progesterone. He added that the immune function could also be affected by suppression, leading to "increased inflammation."
"These changes in hormones and the immune system can lead to increased sebum (oil) production, skin inflammation, and also changes in microbiota, which is the bacterial composition of the skin," he said.
He shed light on how the alteration of the sex hormones level could affect the human, where there would be an increase in testosterone level.
"These changes lead to increased sebum production of the skin and changes the skin microbiota, favouring growth of more virulent bacteria, such as Cutibacterium acnes," he said.
Dr Felix added that the changes in sebum and increase in population of the bacteria would eventually lead to formation of acne, among other possible skin conditions aggravated by existing conditions such as eczema.

He further said that changes in cortisol levels would lead to increase in inflammation, aggravated by suppressed immune functions, exacerbating diseases related to the latest such as eczema and psoriasis. "Both these diseases have dysfunctional immune system, while the changes in microbiota would make them worse with the increases barrier defect of the skin from the changes of skin pH," he said.
In consequence, he said that people would experience dryness of the skin which would further aggravate psoriasis and eczema.
Furthermore, aside from just the testosterone levels increasing from the hormonal alterations from chronic stress, steroid hormone cortisol, alongside oestrogen and progesterone and thyroid hormones would be altered.
"This process leads to disequilibrium in the outer layer of the skin, immune dysregulation in the dermal layer of the skin and increased inflammation and changes in all the functions of the skin appendages," he said.
He added that with changes in skin microbiota and skin microenvironment, there would be major changes in the barrier function of the skin.

Dr Felix said that the healing process would need a good immune system and balanced hormones with the correct proportion of the microbiota.
If not, he said that the condition would worsen over time, causing reduced productivity at work and higher medical leave.
"Individuals with eczema will have frequent eczema flares with more difficult-to-control eczema," he said, adding that a higher rate of infection is also observed in the patients.
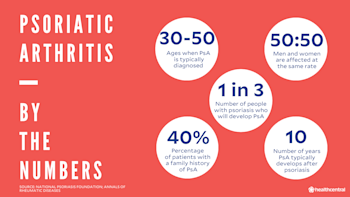
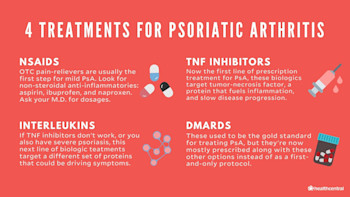
He said that the young adults affected by chronic stress would have severe acne, psoriasis would flare and would spread, potentially leading to psoriatic arthritis, which is a joint disease related to psoriasis.
"All these will propagate themselves as flare-ups of skin diseases, which will cause problems with sleeping, itching, low self-esteem, depression, and many other psychological distresses that in themselves propagate the diseases," he said.
Advocating for actively managing stress on a daily basis, he said that people would need to adopt both psychological and behavioural approaches, which could be done by adopting a good balanced diet, drinking plenty of water, regularly exercising, and having proper sleep to mitigate the adverse effects of the stress.
He emphasised the importance of using appropriate facial products for acne-prone skin, such as non-comedogenic products, and early visit to the doctors could be considered to treat infection of the skin early and not let it become worse.
"Maintaining good barrier function and skin microbiota by using gentle cleansers, patting skin dry after taking a bath/shower, avoiding scrubbing the skin, and maintaining regular moisturisation of the skin is important," he concluded.